Preserve Life — Airway — Assess risk for harm Prevent Further Harm — Breathing — Be there Promote Healing — Circulation — Continue support
Preserve Life — Airway — Assess risk for harm Prevent Further Harm — Breathing — Be there Promote Healing — Circulation — Continue support
Assess for risk of suicide and/or self-harm- Listen non-judgmentally
- Give reassurance or information
- Encourage appropriate professional help
- Encourage self-help and other strategies
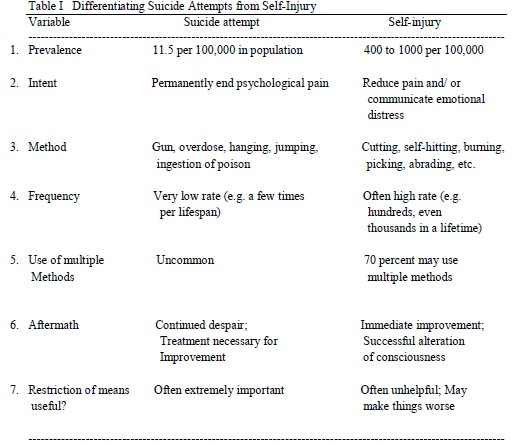
In order to properly help someone distressed, self-harming, or considering suicide, it is important to have at minimally a basic understanding of what the person is going through. Wanting to help is wonderful and welcomed – however misguided attempts at helping can result in serious psychological and physical damage. Understanding the mentality behind self-injury is essential and the right way to effecting positive change. If you don’t think you’re the person for that, turn to someone that not only you know and trust but whom the person you want to help knows and trusts as well. Your attitude is crucial to how things are going to go down. Self-harm is a way of expressing and dealing with deep distress and emotional pain. As counterintuitive as it may sound, for some self-harm is a coping mechanism – a way to feel better. In fact, it may feel so much better that some people may become addicted to it and come to a point where they can’t stop. Those who self-harm ARE NOT ATTENTION SEEKING. In fact, more often than not, people who self-harm keep their actions secret. They may experience shame and fear. This can make it very difficult to come forward and ask for help especially in a world harboring preconceived notions of self-harm. It’s also important to note self-harm may be more than cutting or burning; it can also include less obvious means such as driving recklessly, binge drinking, taking too many drugs, and having unsafe sex.
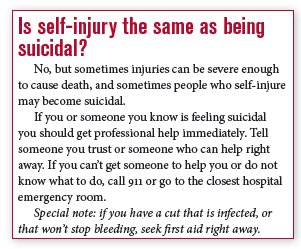 It is a myth that people who self-injure want to die or that self-harm is a failed suicide attempt. The intention is to feel better and usually not out of want to die. They are trying to cope with their pain to go on living. However, studies have shown people who self-harm have a higher risk of suicide than the general population – which is why it’s so important to seek help. Also, don’t assume nor judge for yourself whether the wounds or injuries are minor – seek medical attention. And remember, wounds on the outside may not run as deep as the psychological pain. If you are concerned about someone, let them know you’re concerned. Let them know you want them to be safe, especially for someone who may be experiencing a psychosis. The person may not be open with you at first or even not at all. Try to tailor your approach and interaction to best suit the situation. Be sensitive to the way the person is behaving. If they are avoiding eye contact, give them the space they need. Recognize the person may be frightened of their thoughts, feelings, and of being seen as “different” or “crazy”.
It is a myth that people who self-injure want to die or that self-harm is a failed suicide attempt. The intention is to feel better and usually not out of want to die. They are trying to cope with their pain to go on living. However, studies have shown people who self-harm have a higher risk of suicide than the general population – which is why it’s so important to seek help. Also, don’t assume nor judge for yourself whether the wounds or injuries are minor – seek medical attention. And remember, wounds on the outside may not run as deep as the psychological pain. If you are concerned about someone, let them know you’re concerned. Let them know you want them to be safe, especially for someone who may be experiencing a psychosis. The person may not be open with you at first or even not at all. Try to tailor your approach and interaction to best suit the situation. Be sensitive to the way the person is behaving. If they are avoiding eye contact, give them the space they need. Recognize the person may be frightened of their thoughts, feelings, and of being seen as “different” or “crazy”.
So you suspect someone is self-harming or suicidal. Or they have come to you for help. What do you do?
- Approach the person about your concerns/Let them know they can talk to you. The only way to know for sure how someone is feeling is to ask. Talking about it doesn’t encourage suicidal or self-harming behavior. It has just the opposite effect more often than not (of course like everything there are exceptions to the rule). Asking someone how they are feeling often lowers their anxiety in the long term. Your openness and concern may reflect itself in the person, allowing them to talk confidently, feel less isolated – maybe even relieved. Choose a suitable time and place where you are both comfortable and available to talk without interference. Don’t pressure the person. Respect them – talk to them with the respect and dignity you’d want for yourself.
- Always be aware of your surroundings. Don’t corner or trap the person. When a person is hurting they may already be experiencing high emotions and be on the defensive. It’s not you necessarily – its our natural fight or flight response to stressful situations. Sit next to the person like an equal, not towering over them. Speak calmly but not like you’re speaking to an infant.
- Take them seriously. If someone opens up to you, do not get judgmental, horrified, derisive or shocked. Don’t try to minimize what they are experiencing. Allow the person to talk about their beliefs and experiences without speculating or assuming a diagnosis. Remain calm and confident. Do not get emotionally blackmailing. You cannot shame someone into stopping – if you intend to guilt-trip them, or yell at them, then just find someone else to help. You will just do more harm than good, maybe even to the point of having that person drive the behavior underground.
- Educate yourself. Try to understand and be empathetic of the person’s behaviors whether it be self-harm, suicidal ideation, drinking or substance abuse, psychosis or eating disorders, even if you disagree with it. Learn as much as you can by reading books, finding resources online (like this website!), asking a professional or seeking out other RELIABLE sources.
- Be ready to listen to them. Like, REALLY listen. The best thing you can do is be there in a caring, non-judgmental manner. (This will be especially important for step 2).
- Respect the person’s privacy and confidentiality. Don’t go around telling others their business. Trust is what this is all about. It may be a coping mechanism for yourself to joke about it or gossip about it, but you’ll be doing more harm than good. Consider or research professional help together. If you feel the person or yourself is in mortal danger, however, get emergency or medical attention immediately.
- Do not get frustrated and try to make them stop overnight. Remember – this is a coping mechanism that helps the person deal with distress they’ve been experiencing for more than a day. Removing or attempting to remove a coping mechanism without at least attempting to understand the problems is a quick trip downhill.
What if I don’t feel comfortable talking to the person? It’s okay to feel nervous! If you’re hesitant about approaching the person, don’t avoid them. You may find it more helpful, however, to find someone that you both mutually trust. You’ll feel better and the person in distress will get the care they need. What should I say? Focus on empathy not pity, validation not change, understanding not diagnosis. Be open and honest. Some helpful things to say:
- I’m concerned about you
- How long have you been feeling this way?
- Have you spoken to anyone about this before?
- Is something troubling you?
- I’ve noticed you haven’t joined us for _____ lately – are you alright?
- It’s difficult for me to understand exactly what you’re going through but I can see its really distressing you.
- Something seems to be troubling you. Would you like to talk about it?
- I think your health is important – would you like me to help you find a professional/self-help/other support strategies?
What if the person doesn’t want my help/reacts negatively? It’s difficult and practically impossible to predict how a person will react if you approach them with your concerns. Some may be relieved. Some may just brush it off. And others may react very defensively. This may be for several reasons: they aren’t ready to make a change, they fear change, they have trust issues, and/or they don’t see a problem with their behavior. If someone reacts negatively to your concerns, just remind them you care about them and they can come to you whenever they’re ready. Resist the instinct to get angry or offended – you just can’t force help on a person.
The next post in the Mental Health First Aid series will focus on Step 2 – Listening non-judgmentally.
In the meantime, these are some helpful books on the topic of self-harm:
And remember to wear orange on March 1st, Self-Injury Awareness Day: